CMS 2026 Physician Fee Schedule: What's changing in Remote Care Management
Key changes to Chronic Care Management and Remote Patient Monitoring
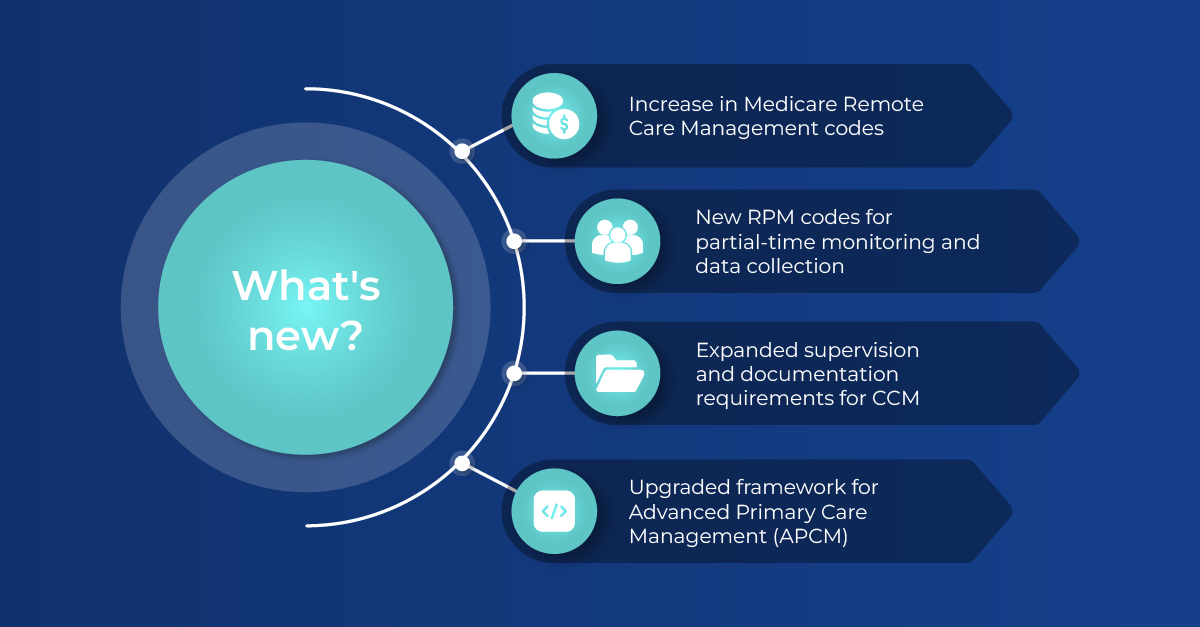
2026 at a glance: What providers can expect
CMS has officially released the Calendar Year 2026 Medicare Physician Fee Schedule Final Rule, and this year’s updates bring some of the most meaningful refinements to care management and Remote Patient Monitoring since the programs began. The changes aim to simplify billing, encourage proactive patient support, and better align reimbursement with the growing role of continuous, longitudinal care.
This article breaks down the major updates across CCM, RPM, and the new Advanced Primary Care Management (APCM) codes, and offers clarity on what practices should expect as they prepare for 2026.
A positive shift in the Medicare Reimbursement Rates
For the first time in five years, CMS finalized an increase in the Medicare payment calculation. The 2.5% increase in payment rate, translating to roughly $1 or $2 more per patient touchpoint, makes remote care programs more financially viable.
For practices with large patient panels, even modest increases in the Medicare reimbursement rate can improve sustainability, and broader adoption of preventive care programs which will result in meaningful improvement in patient outcomes.
Major updates to Remote Patient Monitoring (RPM)
RPM continues to be a key component of value based care, and CMS refined the structure of the program to create clearer pathways and better match reimbursement to clinical effort.
New codes make Remote Care more inclusive and scalable
CMS has introduced a new split for device data collection:
- A new code that captures 2 to 15 days of patient-generated health data (CPT 99445)
- Maintaining CPT 99454 to exclusively capture 16 to 30 days of data
This change represents a significant milestone, as previously, only CPT 99454 allowed billing for 16 days or more of RPM readings. By adding a new code for 2 to 15 days, CMS is expanding the RPM framework to be more inclusive, enabling higher patient reach with different engagement levels. This new code further provides the scalability practices need to grow their care programs efficiently.
New time-based code supports shorter touchpoints
A new first 10-minute RPM Care Management code (CPT 99470) gives clinicians a way to bill for shorter, targeted interventions.. By enabling billing for these shorter touchpoints, this new approach encourages meaningful engagement, supports practices that connect with patients more frequently, and helps patients get the check-ins they need without waiting for longer sessions.
Clarifications and refinements to Chronic Care Management (CCM)
The core CCM structure remains intact, but CMS expanded clarity around supervision and documentation requirements. Time-based billing expectations are more clearly articulated, and practices are encouraged to maintain consistent, team-based communication when delivering CCM services.
The updates help ensure uniformity across different care settings and support ongoing efforts to standardize longitudinal care delivery.
Expansion of Advanced Primary Care Management (APCM)
One of the notable highlights of the Final Rule is the continued development of the Advanced Primary Care Management (APCM) framework.
CMS finalized three new APCM add-on codes that reinforce the importance of behavioral health integration, ongoing care coordination, and comprehensive primary care support. Together, these codes aim to strengthen whole person care while providing a structured, scalable reimbursement pathway for practices looking to expand beyond traditional CCM.
APCM continues to emerge as a central component of CMS’s long-term strategy for preventive care, patient engagement, and value based care.
What the Medicare PFS updates mean for Remote Care teams
Across the Final Rule, CMS is sending a clear message. High-quality care management is essential to improving outcomes, reducing unnecessary utilization, and supporting patients with chronic or complex needs. The refinements in the 2026 rule make the programs more inclusive, scalable, and better aligned with modern patient engagement practices.
Practices that already have established care management workflows will find the transition smooth. Those looking to expand or begin care management programs may find 2026 an ideal entry point, given the clearer rules and additional reimbursement structure.
Exciting changes ahead: Medsien locked in for day-one launch
It is worth noting that Medsien will roll out every required update to CCM, RPM, and APCM within the platform and Care Partner workflows before the Calendar Year 2026 Medicare Physician Fee Schedule Final cycle begins. Thanks to Medsien’s advanced technological infrastructure and automations, all billing automation, device logic, reporting engines, and care management prompts will reflect the new standards from day one, ensuring a seamless transition for partners. Together, these updates raise the standard of patient care and create a smoother, more meaningful experience for both patients and providers. If you have questions about how these changes may affect your practice, reach out to us anytime. We’re happy to help.
More from our blog

2026 updates for RPM, RTM and APCM CPT codes

How recent healthcare policy changes highlight the value of Medsien’s Remote Care Management services

Remote Patient Monitoring under scrutiny: Why Medsien stands out in an evolving landscape

2024 CMS Update Spotlight: Expansion of RPM and RTM to FQHCs and RHCs

Reimagine remote care management
Join our robust and rapidly growing community of leading organizations

